The RECOVER Act: How a Delaware Shell Company Spent $1.5M to Gut VA Mental Health Standards
The RECOVER Act: How a Delaware Shell Company Spent $1.5M to Gut VA Mental Health Standards
By Tbird Tbird’s Quiet Fight | January [DATE], 2026
The Gist
A Delaware shell company spent $1.5 million lobbying for the RECOVER Act—legislation that hands $60 million to private mental health clinics while eliminating quality standards. The shell company is reportedly a front for billionaire Steven Cohen’s 22-clinic network.
What the bill does: Requires only ONE staff member per clinic to have military training. No suicide prevention training. No accreditation. No outcome measurement. Clinics get federal grants + bill insurance + bill VA for the same services. Veterans bypass VA authorization entirely.
The damage: Your mental health gets treated. Your disability claim gets denied. Because private providers won’t know how to document for VA raters.
Cohen tried this in 2017. VSOs killed it. He’s back with better camouflage.
I read the bill line-by-line against existing VA law. Here’s what they’re doing.
The Setup
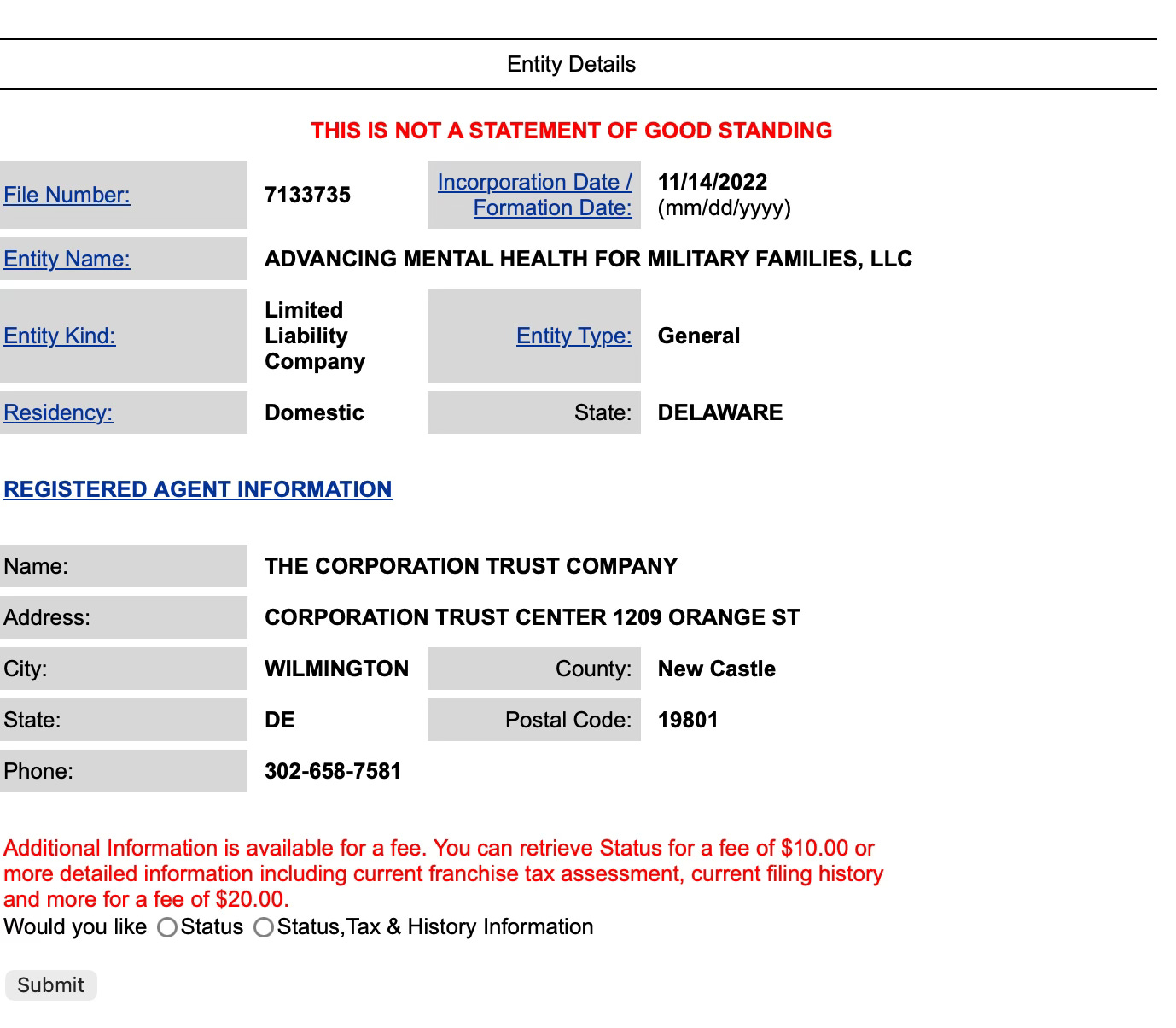
A Delaware shell company with no website just spent $1.5 million lobbying Congress to gut quality standards for veterans’ mental health care. The company—”Advancing Mental Health for Military Families LLC”—is a mailbox.
According to The American Prospect’s investigative reporting, it’s a front for hedge fund billionaire Steven Cohen, whose 22-clinic network stands to collect tens of millions in federal grants if the RECOVER Act passes.
I’ve seen this playbook before. In 2017, Cohen tried the same move with different window dressing. Major VSOs killed it. This time he’s hidden the fingerprints better, but the con is identical—and the regulatory damage is worse.
I read H.R. 2283 against Title 38. It's deliberate: dismantle oversight, wrap it in compassionate language, hope nobody notices.
The Regulatory Breakdown
Part 1: The “Culturally Competent” Loophole
What the RECOVER Act Says:
Bill requires “culturally competent, evidence-based mental health care”
Subsection (f) requires Secretary to establish “requirements” for cultural competency training
Only requirement: “at least one clinician employed by the provider at each facility” must be trained
What This Actually Means:
ONE person per clinic needs training
No definition of “culturally competent” in the bill
No specific training standards
No requirement for veterans-specific military cultural competency
What Current VA Law Requires:
38 USC 1703 (MISSION Act) references “veteran cultural competency” training available through VHA TRAIN program. Under current community care contracts, providers must demonstrate:
Understanding of military culture
Knowledge of service-connected conditions
Familiarity with VA disability rating process
Training on military sexual trauma (MST)
Understanding of combat-related PTSD presentations
The Gap:
The RECOVER Act’s “one person” requirement means 99% of clinic staff could have zero understanding of military culture. Compare this to VA requirements where ALL mental health providers complete annual military cultural competency training.
Part 2: The “Evidence-Based” Shell Game
What the RECOVER Act Says:
Requires “evidence-based mental health care”
No definition of what constitutes “evidence-based”
No requirement that providers be trained in evidence-based practices
No specification of which evidence-based practices
What VA Actually Requires:
38 CFR 4.130 references DSM-5 as the standard for mental health diagnosis. VA mental health providers must be trained in specific evidence-based treatments:
Cognitive Processing Therapy (CPT) for PTSD
Prolonged Exposure (PE) therapy
Cognitive Behavioral Therapy for Insomnia (CBT-I)
Dialectical Behavior Therapy (DBT)
Evidence-based suicide prevention protocols
The Regulatory Problem:
Without specifying evidence-based practices or requiring provider training, “evidence-based” becomes meaningless. Any provider could claim they use “evidence-based” approaches without actual training or fidelity to protocols.
Part 3: What’s Missing
No Accreditation Required:
VA facilities must meet Joint Commission or CARF standards
RECOVER Act grantees: No accreditation requirement
No Peer Review:
VA mental health: Mandatory semiannual peer review
RECOVER Act grantees: No peer review mandate
No Suicide Prevention Training:
VA providers: Mandatory annual suicide prevention training
RECOVER Act grantees: Zero requirement (despite bill prioritizing “high-risk” areas)
No Timeliness Standards:
VA community care: Wait time standards under 38 CFR Part 17
RECOVER Act grantees: Could have longer wait times than VA
No Outcome Reporting:
VA: Tracks and reports symptom improvement
RECOVER Act grantees: No outcome measurement required
No Record Sharing:
VA/Community Care: Integrated health records
RECOVER Act: Veterans bypass VA entirely, creating fragmented care
The Money Scheme
The RECOVER Act provides $1.5 million grants per recipient ($60 million total over three years). Multiple awards per recipient allowed.
Notice what’s missing? Any requirement to increase veterans served.
Bill says grantees can’t charge veterans fees, can’t refuse care based on inability to pay. Says nothing about demonstrating you’re serving more veterans than you would without the grant.
The triple-dip (Section 2(c)(3)):
“Nothing in this subsection shall prevent the recipient of a grant under the pilot program from seeking or receiving reimbursement for all, or a portion, of the mental health care provided to a veteran, including reimbursement under a health plan contract, the Community Care Program of the Department under section 1703...”
Translation:
Veteran with insurance:
Clinic gets: $1.5M federal grant
Bills veteran’s insurance: $150/session
Bills VA under community care: Additional payment
Three payments. Same service.
Veteran without insurance:
Clinic gets: $1.5M federal grant
Bills VA community care: Payment per service
Two payments. Same service.
Optimization:
Serve same veterans you’d serve anyway
Get paid three ways
Zero requirement for expanded access
Zero outcome accountability
Compare this to actual VA grant requirements for homeless services, housing, employment. Recipients must demonstrate: number served, outcomes achieved, cost per veteran, community need, VA coordination.
RECOVER Act requires none of that.
Show us you’ve operated a clinic for three years. Promise to follow undefined “cultural competency” with one trained person. Here’s $1.5 million per facility.
The Pattern
March 2024: VA announces 10,000 position cuts through attrition
June 2024: Frontline clinical jobs cut despite exemption promises
2024: Bost introduces Veterans’ Mental Health Access Act (H.R. 9427)
January 2025: Federal hiring freeze impacts VA
March 24, 2025: Bill reintroduced as RECOVER Act (H.R. 2283)
March 2025: VA plans 80,000+ job cuts (17% workforce reduction)
Present: Veterans experience longer mental health wait times
Standard privatization playbook: Gut VA clinical capacity. Wait for access problems. Offer private “solution” with taxpayer funding and zero oversight.
I’ve watched this for 29 years.
2017 quote from former VA official: “If you start trying to carve into government money in veterans’ care to feed things like the Cohen Veterans Network, that’s actually privatization. It’s going to be death by a thousand cuts.”
RECOVER Act is one cut.
But it establishes precedent. If Congress passes legislation creating a parallel mental health system with no VA oversight and minimal standards, what’s next? Parallel primary care? Specialty care? Inpatient?
Each one chips away at VA’s integrated model.
Why This Matters for Your Claim
You’re filing for PTSD. You need mental health treatment. New clinic opens under RECOVER Act. Free. Closer than VA. You go.
Here’s the problem:
VA mental health providers document for claims purposes. They know what VA raters need to see:
Frequency of symptoms
Severity scaled to rating criteria
Duration and persistence
Impact on occupational and social functioning
Nexus to service-connected condition
Private providers funded by RECOVER Act don’t.
They’ll document that you’re “improving” or “stable” or “progressing well in treatment.”
Three years later, you file your claim. C&P examiner reads records from RECOVER clinic. Sees “patient responding to treatment, symptoms managed.”
Claim denied. Not severe enough. Treatment working.
You just documented yourself out of benefits because your provider didn’t know they were documenting a claim.
What Resistance Looks Like
In 2017, when Cohen tried this the first time, major veterans organizations killed the bill. They recognized the threat and mobilized opposition.
The VSOs got it right. When VFW, DAV, American Legion, and Vietnam Veterans of America say a bill threatens VA healthcare, listen.
This time Cohen spent $1.5 million through a Delaware shell company to hide his involvement. The bill has crept through with less scrutiny.
But it’s the same threat.
The Bottom Line
I’ve compared H.R. 2283 against existing law. I’ve shown you exactly what’s missing and why it matters.
Now the question is: What are you going to do about it?
Call Congress. Contact your VSOs. Share this article. Make noise.
Because if we’re silent, we’re complicit.
And I’m done being silent about schemes that threaten veterans’ healthcare.
UPDATE [Date]: I’ll track the status of H.R. 2283 here, including any scheduled hearings, markup sessions, or votes. If you want notifications when this bill moves, subscribe to legislative alerts.
Resources
Primary Sources:
H.R. 2283 Full Text - RECOVER Act
38 USC 1703 - Veterans Community Care Program
38 CFR 4.130 - Mental Disorders Rating Schedule
38 CFR Part 17 - Veterans Community Care Program Regulations
Investigative Reporting:
The American Prospect: “A Billionaire Tries Again to Hijack Veterans’ Care” (Russell Lemle and Jasper Craven, January 12, 2026)
VA Job Cuts:
VA Plans to Cut 10,000 Jobs (Military.com, March 19, 2024)
Frontline VA Jobs Cut (CNN, June 10, 2024)
5 Reasons Federal Cuts Hit Veterans Hard (PBS, March 17, 2025)
Take Action:
Tbird is a Navy veteran (VAQ-34, 1983-1990) and founder of HadIt.com, a veteran-run VA disability claims knowledge base established in 1997. She publishes investigative journalism and policy analysis at Tbird’s Quiet Fight on Substack.
I use AI as a research and editing assistant—the same way I'd use a good reference book or a sharp editor. Every word published here is reviewed, verified, and approved by me. The perspective, accuracy, and editorial decisions are mine.